Within the intricate network of the human body, there exists a phenomenon known as dorsal vagal shutdown, a term that may sound intimidating but holds significant importance in understanding the body’s responses to stress and trauma. In this article, we delve into the complexities of dorsal vagal shutdown, exploring its mechanisms, implications, and potential therapeutic approaches.
What is Dorsal Vagal Shutdown?
Dorsal vagal shutdown refers to a physiological response mediated by the dorsal vagal complex, a component of the autonomic nervous system responsible for regulating various bodily functions, including heart rate, digestion, and respiratory activity. This shutdown occurs in situations of extreme stress or trauma, wherein the body perceives a threat and activates its defense mechanisms.
Mechanism of Dorsal Vagal Shutdown
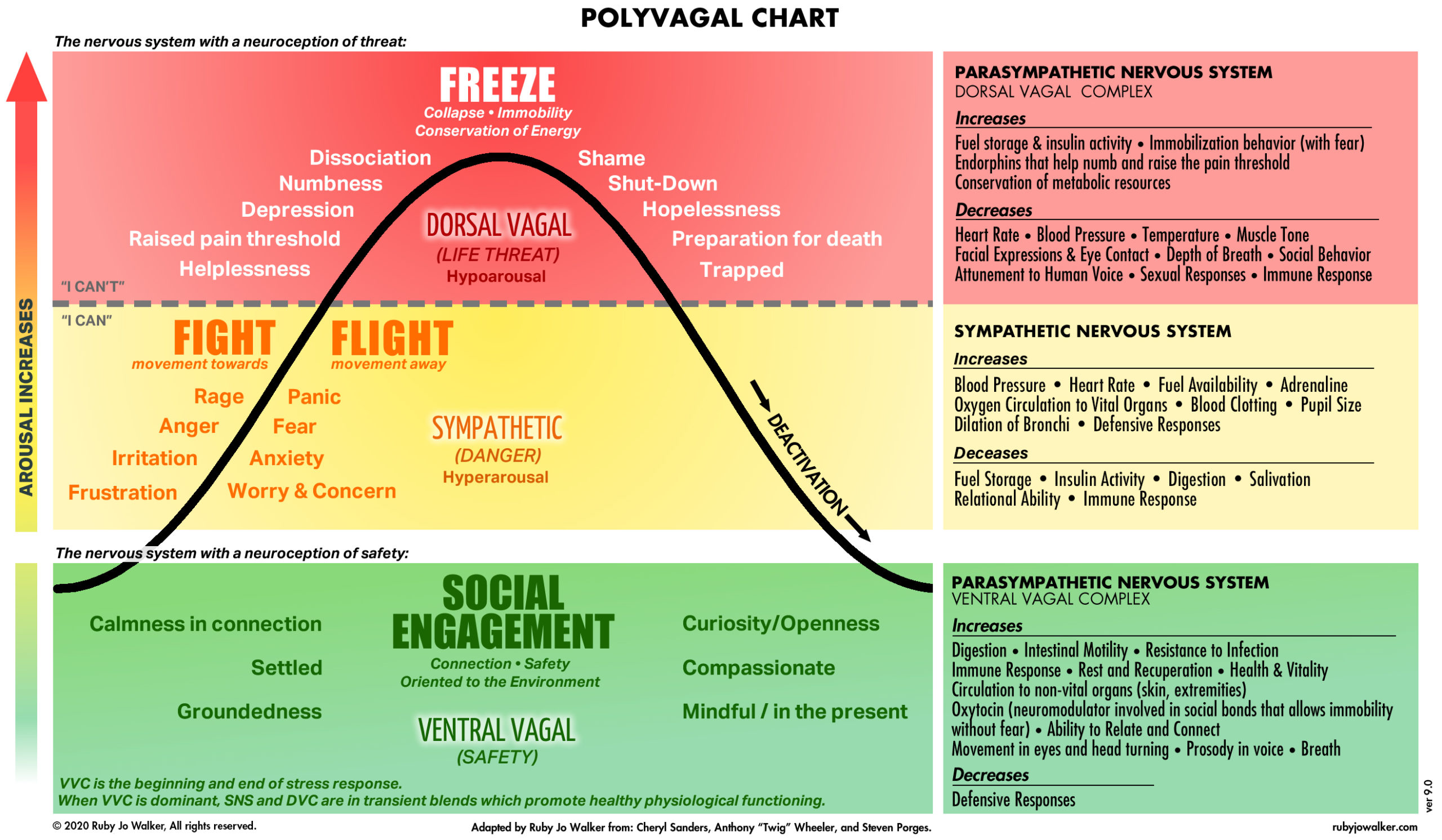
To comprehend dorsal vagal shutdown, it’s crucial to grasp the broader context of the autonomic nervous system (ANS). The ANS consists of three main branches: the sympathetic nervous system (SNS), the parasympathetic nervous system (PNS), and the enteric nervous system (ENS). The PNS has two divisions: the ventral vagal complex and the dorsal vagal complex.
During stressful situations, the sympathetic branch of the ANS initiates the well-known “fight or flight” response, preparing the body to confront or escape the perceived threat. However, if the threat persists or overwhelms the individual, the dorsal vagal complex can override the sympathetic response, inducing dorsal vagal shutdown.
In dorsal vagal shutdown, the body enters a state of immobilization or collapse, characterized by a decrease in heart rate, blood pressure, and metabolic activity. This response is evolutionarily conserved and is believed to have emerged as a survival mechanism in situations where fighting or fleeing is not feasible.
Implications of Dorsal Vagal Shutdown
While dorsal vagal shutdown may serve a protective function in acute life-threatening situations, its chronic activation can have profound implications for physical and mental health. Individuals who experience recurrent or prolonged episodes of dorsal vagal shutdown may develop symptoms associated with various medical conditions, including but not limited to:
- Post-Traumatic Stress Disorder (PTSD): Dorsal vagal shutdown is intricately linked to trauma and can contribute to the development of PTSD, a debilitating psychiatric disorder characterized by intrusive memories, hypervigilance, and emotional numbing.
- Depression and Anxiety Disorders: Dysregulation of the autonomic nervous system, including dorsal vagal shutdown, has been implicated in the pathogenesis of mood and anxiety disorders. Chronic stress can disrupt the balance between sympathetic and parasympathetic activity, contributing to the onset or exacerbation of these conditions.
- Gastrointestinal Disorders: Given the role of the dorsal vagal complex in regulating digestive processes, dysfunction in this system can manifest as gastrointestinal symptoms, such as irritable bowel syndrome (IBS), gastritis, and functional dyspepsia.
- Cardiovascular Complications: Prolonged dorsal vagal shutdown may lead to cardiovascular complications, including bradycardia (abnormally slow heart rate), hypotension (low blood pressure), and increased susceptibility to arrhythmias.
Therapeutic Approaches
Addressing dorsal vagal shutdown requires a comprehensive approach that targets both physiological and psychological factors. Some therapeutic interventions that may be beneficial include:
- Trauma-Informed Therapy: Psychotherapeutic modalities, such as trauma-focused cognitive-behavioral therapy (CBT) and eye movement desensitization and reprocessing (EMDR), can help individuals process traumatic experiences and regulate their autonomic nervous system responses.
- Mind-Body Practices: Techniques such as mindfulness meditation, yoga, and deep breathing exercises can promote relaxation, reduce stress levels, and enhance parasympathetic tone, potentially mitigating dorsal vagal shutdown.
- Medication: In some cases, pharmacological interventions may be warranted to address symptoms associated with dorsal vagal shutdown, including antidepressants, anxiolytics, and medications targeting gastrointestinal motility.
- Lifestyle Modifications: Adopting a healthy lifestyle that includes regular exercise, adequate sleep, nutritious diet, and stress management techniques can support overall well-being and contribute to autonomic nervous system balance.
Conclusion
Dorsal vagal shutdown represents a fascinating yet complex aspect of human physiology, reflecting the body’s adaptive responses to stress and trauma. While this mechanism can offer protection in acute situations, its dysregulation can have far-reaching consequences for physical and mental health. By gaining a deeper understanding of dorsal vagal shutdown and implementing targeted therapeutic approaches, we can strive to restore balance to the autonomic nervous system and promote resilience in the face of adversity.